TIPS TO TREAT YOU BACK PAIN
Most people will get back pain in their lives. The statistics are staggering. It is estimated that over 80% of Australians will suffer from back pain during the course of their lives and 10% will experience significant disability as a result[i]. Back pain disrupts individual’s quality of life and accounts for enormous cost to the community. I tell patients, you only want back pain once in your life, and if you've had it (like myself) you know why.
People who have back pain strive to find a treatment to help them solve the problem. They either have a CT scan or MRI to solve the mystery of back pain.
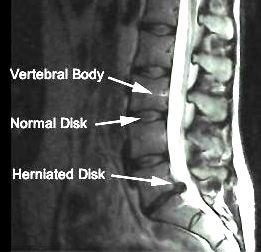
This can be a 2 fold effect:- 1. You may never have a definite diagnosis. In the 1991 New England Journal of Medicine they found 85% of back pain cases have no definitive diagnosis[ii]. This is backed up by another article in the New England Journal of Medicine in 1994 Jensen and colleagues did a MRI on 98 people who were pain free[iii]. They found 52% had a disc bulge at one level, 27% had a protrusion, and 1% had a prolapse. 38% had multi level disc problems. Combined 82% of the patients had one disc bulge or another and they were all pain free. The MRI or CT is only one piece of the clinical puzzle. Imaging deals with how the structure looks not the function of that structure. As I say to my patients, we treat the person not the scan.
I have had patients with a terrible operation report with marked degeneration in their knee or shoulder but can still squat pain free and still lift their arm above their head. Now with this type of information you can have a glass half full or half empty approach.
The half empty approach would say we are close to anatomical failure and are on the verge of getting injured. The half full say we are good let’s just keep on doing what we are doing.
As a physiotherapist I have an unhealthy bias that everyone is going to get injured so I'm trying to find some middle ground. We all have to be careful how we move, how much mobility we have and how much strength and stability we have for a given task.
I'm sure we have all heard stories about "I don't know how I injured my back, I was just putting on my socks or I was just bending to pick something from the floor." These are some of the stories I hear and I put these patients in the half empty category. The people who were close to failure and one more episode of disc stress was the straw that broke the camel’s back.
The glass half full part of me then says "ok you have a disc bulge, lots of people have disc bulges, let’s get you moving right, reduce the disc load and get you back to recovery." That’s how we approach things at Grant Street Physiotherapy.
2. The second effect was drawn to my attention after listening to a physiotherapy podcast recently. They stated that in Swedish medical system they requested a MRI on all lower back pain patients. You would think this was a good idea, however part of the population who found out they had a disc bulge (which was probably normal) started to catastrophise about their condition and developed anxiety, stress and chronic pain problems. Sometimes knowing too much can be a bad thing.
Thanks to Eric Cressey for his great insight into injury management and rehabilitation. His ability to connect the dots and making complex information much easier to understand. [i] 1.Briggs,A. & Buchbinder, R. Back pain: a National Health Priority Area in Australia? MJA 2009; 190 (9): 499-502
[ii] Deyo, RA. Fads in the treatment of low back pain. N Engl J Med. 1991 Oct 3;325(14):1039-40.
[iii] Jensen MC, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med.1994 Jul 14;331(2):69-73.
How do we go about treating back pain?
When you suffer a back injury the pain is shocking. It seems like every movement you make send a sharp stabbing pain in your back. So the first thing is from you and your therapist is don’t freak out. With the right diagnosis and treatment it will generally get better.
1: Avoid Aggravating Acitvities
Avoid the movement in the spine that gives you pain. For the majority of patient this is spinal flexion (bending forward). This may also be the activity that brought about the injury in the first place. Bending to pick something of the floor, making the bed tying up your shoe lace etc.. Therefore it reasonable to assume to avoid this position to give the disc and joint some time to heal. You don’t think of this for your spine but makes more sense for other parts of your body. For e.g. if you have just sprained your ankle you would avoid uneven ground. The difficult part with the spine is that the flexion movement may not be painful straight away but really painful afterwards. The spine can only tolerate so many cycles of bending before it becomes symptomatic, so best thing is to avoid it as much as possible. Dr. Stuart Magill is a spine biomechanist in Canada. He treats patients in a clinic but also examines the mechanical properties of spine in his lab. He has examined how many flexion cycles a spine has by placing a pigs’ spine in one of those sit up machine which is mechanically activated and counts how many bending cycles the discs have until one of them ruptures. The spine can tolerate compression OK but not bending forces.
2: Hip Hinge.
This is where we teach the hip hinge. The hip hinge allows the trunk to bend forward but the movement is coming from the hips and not the spine. In this way we are sparing the spine from load and distributing it to the hips. Magill has measured that the spines bending forces are reduced by 30-40 % when using the hip hinge position. I feel this is really important in the initial stages so the patient can reduce the amount of mechanical load on the spine and give it a chance to recover.
Hip Hinge Demonstration
3: Avoid Bending
Avoid bending and sustained flexed postures. Examples of these are sitting, mopping/sweeping, ironing, preparing food and manual tasks which are repetitive and make you stand in the one position for long periods. There is no one perfect standing or sitting posture. We recommend changing position regularly to avoid mechanical load in one specific area. It’s like sitting on a hard wooden chair, you can tolerate it for a while but then the pressure gets too much and you need to change your position. The trick is to change position before your back gets sore.
4: Pain killers and Anti inflamatories
Take some anti inflammatory medication (NSAIDS) like nurofen or voltaren and adequate pain relief. The NSAIDS can take the edge of the pain and restrict irritation to help you move and sleep a little better. Even if you have tried them before, try them again in conjunction with some therapy and with the above advice. Make sure to ask the chemist if they are OK to take with any current medication you are taking or with any other health problems you may have.
5: What exercises should I do?
If it is bending forwards that gives you most of the pain and going backwards is just stiff we suggest some bending backwards movements. In other words if you are flexion intolerant we want to reverse this load on your discs and encourage bending backwards. We all live in a flexed posture. Wake up sit down for breakfast, drive 30 minutes to work, sit all day in front of a computer, drive home and then sit on a bike for exercise. To counteract this, stand up regularly and reverse these postures by bending backwards. Now this is not for everyone who has a disc problem. It can make you worse and needs to be correctly prescribed to your movement disorder. If the referred pain gets worse or your back pain gets worse this is not for you. Below is a video by Dr Liebenson, a well known therapist in the U.S.A. and author of Rehabilitation of the Spine describing this flexion intolerant patient and the extension exercise lying on your stomach. Not everyone has time to do this; this is why I suggest the standing version for ease and compliance. The other benefit of this exercise is that it stretches out the front of your hip joint and the hip flexor muscle that cover it.
6: Regional Interdependance
Next we look at the joints below and above. Namely the thoracic joints and the hip joints. In the hips the hip flexors and rotators get tight. If the hips are not working right they get restricted when you extend the hip while you walk and restricted in flexion when you bend. This means the movement comes from your lower back. The thoracic joints for most people are stiff and we recommend to loosen these up. If the hips and thoracic joints don’t move the movement has to come from somewhere else. When you have back pain you want to reduce the load around these areas to reduce pain and give the area a chance to heal. For me this is simple mechanical loading problem, restricting movement in an injured area by mobilising joints above and below to share the load. Everybody wants to strengthen the area first, but it is no good if you have faulty movement patters from areas which cannot move.
7: Massage and heat
When you get a back injury the muscles and fascia of the tissue spasm to splint the area. They become tight as a drum and can cause pain in itself rather than the injury. The spasm also causes restriction in movement, and any movement you try to make grabs like all hell. This makes it hard to regain normal movement and normal movement patterns. We find massage and heat works well to relax these muscles and reduce tone in the back, and l hip muscles. Not all massage is created equally. The fascia of the body is connected in different lines around the body. A great book called Anatomy Trains by Thomas Myers outlines these fascial lines oand the connections of these lines. You can effect tension in one area by massaging other areas to reduce load on the tissue. This requires a different technique of massage to change the fascia and knowledge of where these fascial lines run and their best access points.
|
3 tips for treating neck pain
The first question I ask myself is how does the neck injury start in the first place? This is the question you ask yourself for any injury. One day you are normal the next day you have pins and needles down your arm and can’t turn your head. Injuries in most part are small cyclical stresses that build up over time stressing the discs, muscles and joints which lead up to their ultimate structural failure and cause pain. Otherwise known as arthritis. A term which I don’t really like because the patient then thinks of this as a disease. Something that is genetically inherited because their mum also had arthritis. Arthritis is just degeneration (wear and tear) on a particular structure. Like we have mentioned before there are studies that show we have degeneration but we don’t feel any pain. Too many times therapists look locally just at the neck and do not focus on the cause of the neck pain.
That said here are my top 3 tips for treating neck pain
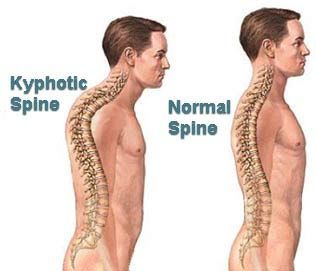
Tip 1. POSTURE
Everyone probably hates hearing about this, but it plays the number 1 key role in developing neck pain. It is just pure engineering and stress points, not rocket science. As you can see from the picture above a curve in the upper spine (commonly known as a kyphotic curve) places the head in a more forward position. This automatically puts a stress point on the base of the cervical spine. The head weighs 8-10kg which requires the muscles around the neck to work harder than they should to stop the head from falling forwards. When the head is tilted forward what you can see from the picture is the head and eyes now look down. The body compensates by tilting the neck upwards so the eyes can now look at the horizon. This puts a kink in the middle of the cervical spine and this is where most degenerative changes occur in the neck. This is how important posture is to neck health and recovery of your injury.
Step 2 Thoracic Spine Mobility
Thoracic spine mobility drills is the first step in improving posture. This area in between your shoulder blades gets locked down and very stiff. The example I give my patients is they get up to go to work sit down for breakfast. Drive the car to work for 45 minutes then sit down at the desk in front of their computer 8 hours, drive home again, sit on the couch and watch T.V, or for the more energetic get on a bike and exercise. The majority of the time is sitting down getting more and more stooped. This area never gets stretched and as a result our posture suffers over time.
Tip 3 Stretch the anterior shoulder and chest muscles.
As a result of a stooped posture you are also going to get tight chest muscles. Rounded shoulders tight chest muscles go hand in hand. An easy exercise is to stretch into a door frame. Put your arms in the high 5 position in the doorway and lean forward. We try and cue the exercise to also feel the stretch in the thoracic area. Some can compensate for a lack of movement by extending their lumbar spine. We encourage you to pop your chest out and stiffen the abs a little to focus the stretch more in the chest and the mid back area. You can also tweak this up by doing it on the floor. Place a rolled up towel down your spine. Lay down on it and place your hands in the high 5 position and try and get your arms to touch the ground. Now you are getting the best of both worlds by targeting the chest and the thoracic area. This exercise is great for most people. However if you have really loose (hyper mobile) shoulders you tend to stretch more the shoulder joint than the thoracic area. If you can get your body way through the door jam your shoulders may be the structure stretching too much. |